Magnesium Deficiency Symptoms and Practical Tips to Manage It
Magnesium deficiency symptoms can often be subtle, making this little-known condition a “silent epidemic.” Yet even mild magnesium deficits can manifest in a surprising range of signs—from muscle cramps and fatigue to mood disturbances and heart rhythm irregularities. In this post, we’ll explore the common indicators of magnesium deficiency and explain why spotting them early—and boosting your magnesium intake—is essential for supporting overall health.
What is Magnesium?
Magnesium is a vital mineral that our bodies require for numerous essential functions. It plays a crucial role in muscle and nerve function, blood sugar regulation, and maintaining healthy blood pressure levels. You can find magnesium in a variety of foods, including nuts, seeds, whole grains, and leafy green vegetables. For example, a handful of almonds or a serving of spinach can significantly contribute to your daily magnesium intake.
What is Magnesium Deficiency?
Magnesium deficiency, also known as hypomagnesemia, occurs when the body lacks sufficient magnesium. This deficiency can arise from inadequate dietary intake, certain medical conditions, or the use of specific medications. When magnesium levels drop, it can lead to a range of symptoms that impact both physical and mental health. For instance, someone who has recently undergone gastrointestinal surgery might experience a deficiency due to malabsorption.
What Are the Primary Magnesium Deficiency Symptoms and Signs?
Recognizing the symptoms of magnesium deficiency is essential for maintaining good health. Here are some common signs to be aware of:
Muscle Cramps and Twitches
Muscle cramps are one of the most prevalent symptoms of magnesium deficiency. You might experience sudden, painful contractions in your muscles, particularly in your legs. For example, imagine waking up in the middle of the night with a cramp that makes it difficult to walk. This discomfort can disrupt your sleep and daily activities.
Fatigue and Weakness
Feeling unusually tired or weak can also indicate magnesium deficiency. If you find it challenging to complete your daily tasks or feel drained after minimal effort, it may be time to evaluate your magnesium levels. Picture a busy parent who struggles to keep up with their children’s activities due to constant fatigue—this could be linked to low magnesium.
High Blood Pressure
Low magnesium levels can contribute to high blood pressure. Magnesium helps relax blood vessels, so when levels are low, it can lead to increased pressure in the arteries. For instance, someone who has recently been diagnosed with hypertension might benefit from assessing their magnesium intake.
Irregular Heartbeat
An irregular heartbeat, or arrhythmia, can occur if magnesium levels are too low. This may feel like your heart is racing or skipping beats, which can be alarming. Imagine a young athlete suddenly experiencing palpitations during a workout—this could signal a magnesium deficiency.
Mental Health Symptoms
Anxiety and Depression
Magnesium plays a significant role in brain health, and a deficiency may lead to heightened feelings of anxiety or depression. If you notice changes in your mood or increased stress, it could be linked to your magnesium intake. For example, a college student facing academic pressure might find that their anxiety worsens due to low magnesium levels.
Apathy and Mood Changes
Feeling apathetic or experiencing mood swings can also be symptoms of magnesium deficiency. If you find yourself losing interest in activities you once enjoyed, it might be time to evaluate your magnesium levels. Consider a creative individual who suddenly feels uninspired—this could be a sign of an underlying deficiency.
You need to keep in mind that magnesium deficiency symptoms in kids can result in stunted growth. This further shows that the symptoms and signs of magnesium deficiency can be quite serious. Some conditions associated with this magnesium deficiency include ADHD, depression, chronic fatigue syndrome, epilepsy, migraine, osteoporosis, chest pain, cluster headaches, and even hypertension.
Causes of Magnesium Deficiency
Several factors can contribute to magnesium deficiency, including:
- Low dietary intake of magnesium-rich foods
- Chronic diarrhea or gastrointestinal issues
- Diabetes, which can affect magnesium absorption
- Alcohol use disorder, which can lead to lower magnesium levels
Diagnosis And Treatment of Magnesium Deficiency
Want to know how magnesium deficiency gets diagnosed? Well, you should know that the most common way is through a blood test. If there are low magnesium levels in the blood, then you’ll know that it has become a problem. We are saying this because low magnesium levels can lead to a range of health problems, including muscle spasms, fatigue, and irregular heartbeat.
When we talk about magnesium deficiency symptoms in adults, its treatment often involves magnesium therapy. This will include taking magnesium supplements as soon as you can for up to a month (sometimes more and sometimes less depending on the severity of your condition). In most cases, this is a problem that can easily be solved once you start the recovery regimen.
Treatment Options for Magnesium Deficiency
If you are diagnosed with magnesium deficiency, there are several treatment options available:
- Magnesium Supplements: These can help boost your magnesium levels quickly. Always consult with a healthcare professional before starting any supplements. For instance, a doctor may recommend a specific type of magnesium supplement based on your individual needs.
- Dietary Sources: Increasing your intake of magnesium-rich foods can also help. Foods like spinach, almonds, and black beans are excellent options. Imagine a meal plan that includes a spinach salad topped with almonds and black beans—this could significantly enhance your magnesium intake.
How to Prevent Magnesium Deficiency
Preventing magnesium deficiency is achievable by incorporating magnesium-rich foods into your diet. Here are some tips:
- Eat a balanced diet that includes nuts, seeds, whole grains, and leafy greens.
- Consider magnesium supplements if you are at risk of deficiency, but consult with a healthcare provider first.
The Role of Magnesium in Overall Health
Magnesium is essential for many bodily functions. It helps maintain strong bones, supports muscle function, and even aids in sleep quality. Ensuring you have enough magnesium can lead to better overall health and well-being. For example, individuals who maintain adequate magnesium levels often report improved energy and mood.
FAQ
What are the common causes of magnesium deficiency? Common causes include low dietary intake, chronic diarrhea, diabetes, and alcohol use disorder.
How can I tell if I have a magnesium deficiency? Look for symptoms like muscle cramps, fatigue, high blood pressure, and mood changes. A healthcare provider can perform tests to confirm deficiency.
Are there any risks associated with taking magnesium supplements? Yes, taking too much magnesium can lead to side effects like diarrhea and abdominal discomfort. Always consult a healthcare professional before starting supplements.
Conclusion
In summary, magnesium deficiency symptoms can affect many aspects of your health—from muscle function and energy levels to mood and heart rhythm. Because these symptoms are often overlooked or mistaken for other issues, addressing low magnesium levels early is essential. Fortunately, high-quality supplements can help restore balance quickly and safely. At PrescriptionPoint, we offer trusted options like Jamieson Magnesium, Jamieson Calcium Magnesium with Zinc, and Magnesium Citrate—all formulated to support optimal absorption and effectiveness. If you’re experiencing signs of magnesium deficiency, consult with your healthcare provider and explore these convenient, affordable supplements to help support your overall wellbeing.
References
- NCBI. 2023. The Integral Role of Magnesium in Muscle Integrity and Aging
- Healthline. 2024. Magnesium Deficiency: Symptoms, Recommendations, and More
- Ability Clinic. How Does Magnesium Help Muscles?
- Diabetes Care. 2014. Higher Magnesium Intake Reduces Risk of Impaired Glucose
- Frontiers in Physiology. 2024. Magnesium in hypertension: mechanisms and clinical implications
- WebMD. 2024. Magnesium-Rich Foods: Why Your Body Needs Them
- Ability Clinic. How Does Magnesium Help Muscles?
- Diasporal.com. 2024. Magnesium and cramps
- Healthdirect.gov.au. 2024. Magnesium deficiency – symptoms, causes, treatment & prevention
- Medicalnewstoday.com. 2024. What to know about a magnesium deficiency (hypomagnesemia)
- Diasporal.com. Magnesium and diabetes
- Medlineplus.gov. Magnesium Blood Test
- Sps.nhs.uk. 2024. Treating acute hypomagnesaemia in adults
- Vinmec.com. 2024. Possible side effects of magnesium supplements
Also Read
Discovering Impactful Ways For Type 2 Diabetes Management
7 Game-Changing Tips For Managing Type 2 Diabetes
10 Foods That Reduce Anxiety And The Ones That Worsen It
Recognizing The Silent Gerd Symptoms Beyond Heartburn
Uncovering Top 6 Expert Tips For A Healthy Heart
Laryngopharyngeal Reflux (LPR) – Symptoms, Risk Factors, Causes and Diagnosis

Table of Contents
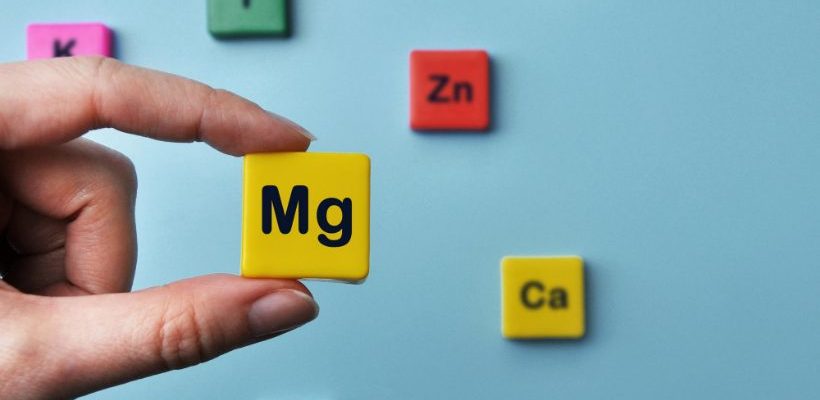
Gastroesophageal Reflux Disease (GERD) is a common condition where stomach acid flows back into the esophagus, but not all cases present with the classic symptom of heartburn. Silent GERD, also known as Laryngopharyngeal Reflux (LPR), can manifest in various ways that are less obvious. Here’s what you need to know about the symptoms of silent GERD.
Silent reflux, also known as Laryngopharyngeal reflux (LPR), is a condition in which stomach acid flows back up the esophagus (swallowing tube) into the larynx (voice box) and throat. LPR is called silent reflux because it often does not cause any symptoms in the chest.
Image courtesy of National Library of Medicine
Symptoms of LPR
Laryngopharyngeal Reflux (LPR) presents in various ways, and identifying these symptoms early is critical for effective management. According to the National Library of Medicine, here are all the possible symptoms of LPR:
- Chronic cough or excessive throat clearing
- Vocal Cord Irritation
- Postnasal drip
- Dysphagia
- Coughing after eating or lying down
- Breathing difficulties or choking episodes
- Throat Sensation
- Throat Discomfort
- Globus sensation
Important: If you are experiencing persistent or severe symptoms of LPR, such as chronic cough, hoarseness, difficulty swallowing, or chest pain, do not delay seeking medical advice. These symptoms can indicate a more serious condition and require proper diagnosis and treatment from a healthcare professional.
Risk Factors
Several factors can increase the risk of developing LPR, but understanding the risks can empower you to make positive changes for your health:
- Obesity and Excess Body Weight – Managing weight can help reduce abdominal pressure and improve overall well-being.
- Hiatal Hernia – A hiatal hernia happens when the top of your stomach bulges through an opening in your diaphragm. Simple lifestyle adjustments can often alleviate symptoms effectively.
- Smoking – Quitting smoking not only strengthens the lower esophageal sphincter but also brings countless benefits to your health.
- Pregnancy – This is a temporary phase, and many find relief through tailored dietary and lifestyle choices.
- Certain Medications – If you suspect your medications might contribute, discussing alternatives with your healthcare provider can make a difference.
- Dietary Choices – Choosing a balanced diet and avoiding triggers like fatty, spicy, or acidic foods can support a healthier digestive system while still enjoying delicious and satisfying meals.
By identifying these factors, you can take proactive steps toward better digestive health and overall wellness.
Causes
The causes of silent GERD are similar to those of GERD but may be more subtle:
- Weak Lower Esophageal Sphincter (LES)
- Hiatal Hernia
- Abnormal Esophageal Contractions
- Delayed Stomach Emptying (Gastroparesis)
- Increased Abdominal Pressure
- Obesity and Excess Body Weight
- Pregnancy
- Smoking
- Certain Medications
- Dietary Factors
When to Contact Your Physician?
If you are experiencing any of the above-mentioned symptoms, it is crucial to contact your physician. They may prescribe medications such as proton pump inhibitors (e.g., omeprazole, esomeprazole, lansoprazole) or refer you to a gastroenterologist for further testing.
Diagnosis
Diagnosing silent reflux is challenging due to the lack of a definitive diagnostic test. Silent reflux is characterized by gastric contents refluxing into the pharynx or larynx, causing symptoms like chronic throat clearing, hoarseness, and a globus sensation. These symptoms often overlap with other conditions, making accurate diagnosis critical yet complex.
Initial Diagnostic Approaches
The process often begins with a consultation involving both an otolaryngologist and a gastroenterologist. Flexible laryngoscopy is a cornerstone test, helping to exclude other laryngeal pathologies like allergic rhinitis or sinusitis. Additionally, ambulatory reflux monitoring is essential to assess esophageal reflux burden. Experts recommend conducting this test without prior acid-suppressive therapy to ensure accurate results. Notably, up to 60% of patients with isolated laryngeal symptoms might not exhibit gastroesophageal reflux disease (GERD), emphasizing the need for tailored diagnostic strategies.
Challenges in LPR Diagnosis
The absence of heartburn or regurgitation in many silent reflux patients further complicates the diagnosis. Patients often undergo multiple consultations and tests before a conclusion is reached. Research indicates that the best outcomes occur when objective findings, such as disrupted anti-reflux barriers or elevated esophageal acid burdens, are present. Despite advancements, identifying true silent reflux cases remains an evolving field that requires further study.
Treatment Options
Once diagnosed, treatment options span lifestyle modifications, pharmacological interventions, and, in severe cases, surgical procedures. The choice of treatment depends on the severity of symptoms and the presence of objective reflux indicators. Further research and clinical consensus are needed to refine the diagnostic criteria and therapeutic pathways for silent reflux.
Potential Complications
If left untreated, LPR can lead to more serious health conditions, including:
- Esophagitis – Esophagitis is the inflammation or damage to the esophagus lining.
- Barrett’s Esophagus – Barrett’s Esophagus is a precancerous condition requiring immediate attention.
- Esophageal Ulcers or Strictures – Untreated LPR can result in painful complications that may affect eating and drinking habits.
Managing GERD symptoms early is the best way to prevent long-term health issues.
Final Words
LPR symptoms can significantly impact your quality of life, but it is manageable with the right approach. Whether you’re dealing with heartburn or silent symptoms, early recognition and treatment are key.
Visit your doctor for proper diagnosis, and consider trusted medications to alleviate discomfort.
Sources:
Krause AJ, Walsh EH, Weissbrod PA, Taft TH, Yadlapati R. An update on current treatment strategies for laryngopharyngeal reflux symptoms. Ann N Y Acad Sci. 2022 Apr;1510(1):5-17. doi: 10.1111/nyas.14728. Epub 2021 Dec 17. PMID: 34921412; PMCID: PMC9012673.
Cui N, Dai T, Liu Y, Wang YY, Lin JY, Zheng QF, Zhu DD, Zhu XW. Laryngopharyngeal reflux disease: Updated examination of mechanisms, pathophysiology, treatment, and association with gastroesophageal reflux disease. World J Gastroenterol. 2024 Apr 28;30(16):2209-2219. doi: 10.3748/wjg.v30.i16.2209. PMID: 38690022; PMCID: PMC11056915.
Smith RE, Sharma S, Shahjehan RD. Hiatal Hernia. [Updated 2024 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562200/
Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.Barrett esophagus. [Updated 2022 Jul 30]. Available from:https://medlineplus.gov/ency/article/001143.htm
Also Read
Magnesium Deficiency Symptoms and Practical Tips to Manage It
5 Ways to Lower Cortisol Levels and Its Symptoms

Going to bed late and getting up early might seem productive in the short term but is not healthy in the long term. The trend of popping an energy drink or guzzling a venti coffee first thing in the morning to deal with the hardships of being perpetually tired can lead to some undesirable health issues.
You need to keep in mind that cortisol and sleep are closely related. If you are among those suffering from constant fatigue or chronic stress, then you may have elevated or high cortisol levels. So, if you want to know how you can lower cortisol levels in your body, keep reading.
What is Cortisol?
Cortisol hormone is a steroid that is produced by the adrenal gland in response to stress. Ordinarily, cortisol is highest in the morning, around 8 am, and then gradually lowers throughout the day, especially after exercise, reaching a low around 4 am, or a few hours after the onset of sleep. The problem with the stress-filled, no-sleep lifestyles of many people is that they don’t get a chance to deplete their levels; in other words, the cortisol stays elevated through the night which clearly means that sleep and cortisol are closely related.
This lack of sleep leads to a cortisol imbalance in the body. With high cortisol levels, the production of testosterone and DHEA are suppressed, the latter two being responsible for many important anti-inflammatory and oxidative functions.
(Since women, however, have less testosterone, a high cortisol-induced drop in their testosterone is normally going to affect women more than men. And for women who want to stay young, lean, energetic, and otherwise active, a healthy level of testosterone is very important. So, keeping the link between cortisol levels and sleep is even more important for women.)
What Are the Symptoms of High Cortisol?
Prolonged high cortisol levels can enact significant physiological changes in both men and women. The symptoms include, but are not limited to the following:
- Exhaustion (reduced physical/mental energy = low vigor)
- Low sex drive
- Decreased muscle mass
- Reduced calorie/fat-burning
- Increased abdominal fat
How to Lower Your Cortisol Levels?
As the name itself suggests, a high cortisol level number simply implies an increase in your cortisol levels. And if you have some or all of the above-mentioned symptoms, you most probably have a cortisol imbalance. But worry not as we are here to make you familiar with the link between cortisol and sleep, and ways to lower cortisol levels. Reducing cortisol and restoring balance in the body is relatively easy. Use any or all of these approaches to help reduce cortisol levels.
Instead of blaming your sleep for cortisol imbalance, it’s better that you pay attention to how you can reduce it to bring it back to normal. Here we are going to tell you about ways to treat high cortisol levels.
-
Exercise:
Just like cortisol and sleep, cortisol and exercise also have a complex relationship, as cortisol levels can be affected by both the intensity and duration of physical activity. Remember that virtually all forms of exercise help to lower cortisol levels. So, find a sport that you enjoy or the best exercise to reduce cortisol and try to get the blood pumping as much as possible each day.
-
Diet
Cortisol imbalance can be treated with the right diet as well because certain foods and nutrients may affect cortisol levels in the body. Fatty or overly sugary, processed foods can affect the adrenal gland in negative ways. So, stick to brightly colored fruits and vegetables, lean meats, and unrefined/whole carbohydrates because they are foods that reduce cortisol.
-
Stress Management:
Just like lack of sleep and cortisol, stress and cortisol are also closely related, as cortisol is a hormone released in response to stress. Stress is a part of life, but how we deal with those stressors at a psychological level will determine our hormonal response, as stress researchers from around the world have determined.
In other words, if you acknowledge stress too much, or with too much intensity, your body will respond in tune with your emotional change. But once you learn to manage stress, it can help in reducing your cortisol levels back to normal.
-
Dietary Supplements:
In addition to, or as part of a balanced diet, there are certain supplements to reduce cortisol and belly fat which can be beneficial to maintaining a proper physiological equilibrium as well. The Malaysian herb Eurycoma longifolia (Tongkat ali) is a potent option for energy and one of the best supplements to reduce cortisol. It can be used as a natural method to help safely lower cortisol levels in the body and restore the body’s hormonal equilibrium.
-
Find A New Hobby
Engaging in a new hobby has the potential to effectively lower cortisol levels. Exploring activities such as painting, gardening, or playing a musical instrument can divert attention from daily worries, promoting relaxation and a sense of fulfillment. This shift in focus allows the mind and body to unwind, leading to decreased cortisol production and an overall reduction in stress levels. So, discovering a new hobby can be a therapeutic pathway towards a calmer, more balanced life.
Final Thoughts
We hope that now you understand the correlation between higher and lower cortisol levels and sleep schedules. Remember that sometimes an increased cortisol level might be difficult to notice. But if not treated at the right time, it can turn into something even more fatal. So, if you feel like your hormones are out of balance, it is best to talk to a doctor immediately to get some medication.
Also Read
10 DANGEROUS EFFECTS OF STRESS ON YOUR HEALTH AND HAPPINESS
7 GAME-CHANGING TIPS FOR MANAGING TYPE 2 DIABETES
DISCOVERING 5 EFFECTIVE WAYS FOR PREVENTION OF ASTHMA
Tips To Maintain an Active Lifestyle with Early Onset Alzheimer’s

We all get to hear about numerous diseases and health issues, some of which affect you while others affect you mentally. If we talk about the issues related to your mental well-being, the first disease that comes to our mind is Alzheimer’s.
Many people lose hope after getting diagnosed with early-onset Alzheimer’s, but do you know that you can deal with it while staying active? Yes, you heard it right! If you want to know more about it, keep reading.
What Is Early-Onset Alzheimer’s?
While studies have shown no cure for early-onset Alzheimer’s disease, its patients are proving that the best treatment for the disease is to stay as active as possible for as long as possible. We know that one question might be coming to your mind: what is early-onset Alzheimer’s? Well, it is defined as those cases diagnosed in people younger than 65.
Moreover, many health practitioners believe that it is quite challenging to diagnose early-onset Alzheimer’s, even if the patient displays clear signs of that disease. Doctors first assume other problems, and it is only through a process of elimination that Alzheimer’s is eventually diagnosed.
Which Individuals Are at Risk of Developing Early-onset Alzheimer’s Disease?
According to research, early-onset Alzheimer’s disease poses a unique set of challenges, particularly for those who are affected at a younger age. While the exact cause remains elusive, several factors increase the risk of developing this condition.
Therefore, risk assessment for early-onset Alzheimer’s can help individuals and their loved ones proactively manage their health.
Here are some common risk factors for early-onset Alzheimer’s:
1. Genetics
As per the studies, a family history of Alzheimer’s increases the likelihood of developing the early-onset form. Mutations in specific genes, such as APP, PSEN1, and PSEN2, have been linked to inherited cases.
2. Down Syndrome
Similarly, people with Down syndrome are more prone to developing early-onset Alzheimer’s due to a genetic predisposition.
3. Lifestyle Factors
Certain lifestyle choices can also impact the risk of developing Alzheimer’s. Chronic conditions like high blood pressure, diabetes, obesity, and smoking have been associated with a higher likelihood of developing the disease at an earlier age.
4. Environmental Factors
Lastly, exposure to certain environmental toxins, such as heavy metals and pesticides, has been linked to an increased risk of developing Alzheimer’s disease. By understanding these population risks of early onset Alzheimer’s, individuals can make informed decisions about their health and take proactive steps to mitigate the risks associated with early-onset Alzheimer’s disease.
Identifying Early-onset Alzheimer’s Disease Through Diagnosis
Now, identifying the disease plays a crucial role in timely intervention and treatment for early onset Alzheimer’s. With advancements in medical science, distinguishing early-onset Alzheimer’s from other conditions has become more accurate. According to experts, innovative diagnostic tools, such as genetic testing and brain imaging techniques, aid in pinpointing the disease’s presence and progression.
Similarly, recognizing the unique characteristics of early-onset Alzheimer’s, such as cognitive decline in younger individuals, enables healthcare professionals to administer appropriate treatments and support. By combining these early-onset Alzheimer’s differential diagnosis approaches, medical experts can provide targeted care, enhance patients’ quality of life, and potentially slow down the advancement of this challenging neurodegenerative disorder.
Genetic Factors Among the Causes of Early-onset Alzheimer’s
Studies have shown that the early onset Alzheimer’s genetic component is a significant factor in the development of this disease. But through genetic tests for early onset Alzheimer’s, healthcare professionals can identify specific mutations in genes like APP, PSEN1, and PSEN2. These mutations contribute to the genetic predisposition of the disease.
However, it is important to acknowledge that not all cases of early-onset Alzheimer’s have a genetic origin. As mentioned above, there are non-genetic early-onset Alzheimer’s factors, including lifestyle choices and environmental exposures, also play a role.
How Are Early-Onset Alzheimer’s Patients Staying Active?
Cindy Kolick, a professional theater actor, first presented early-stage Alzheimer’s disease at the age of 42 and was later diagnosed with early-onset Alzheimer’s disease at the age of 52. Alzheimer’s disease forced her to resign from her profession; nonetheless, she remained as active as possible. She sings in the chorus at the residential complex she lives in, exercises, and participates in online Alzheimer’s drug studies on a daily basis.
Another Alzheimer’s disease early onset case is that of Pati Hoffman. Hoffman used to have a corporate marketing job but was forced to leave it with an early diagnosis at the age of 55. Hoffman now speaks about her struggles at events and continues to stay active by volunteering at the local food bank and walking.
Doctors and nurses also recommend that early-onset Alzheimer’s disease patients join support groups. As Danielle Arends, a nurse practitioner, stresses, Alzheimer’s disease “can be an isolating disease”. A peer support group, staying active, and medication to treat dementia, will aid in the fight against the signs of early-onset Alzheimer’s.
5 Expert Tips to Stay Active with Early-Onset Alzheimer’s
- Daily exercise is essential for promoting both mental and physical health. You should choose something therapeutic and repetitive.
- If you enjoy yoga, make yoga a daily excursion. If you enjoy swimming, take up swimming. If you enjoy walking, go on walks with your dog or your friends!
- Continue doing what you are passionate about, but make sure that you do it on a smaller scale. In Kolick’s case, this meant continuing singing, just not at the professional level; while in Arends’ case, she continues to fulfill a leadership role by speaking at conferences and events about her personal struggles.
- It goes without saying that early-onset Alzheimer’s requires medical treatment – both therapy and medicine. So, you should follow the directions given by your doctor and take whatever dementia medication is prescribed.
- Attend personal counseling sessions and peer support groups.
Conclusion
All in all, we can say that Alzheimer’s is a disease that affects you mentally, but you can fight it by staying active. Keeping a positive mindset and some exercise is all you need to navigate a healthy and happy lifestyle while suffering from early-onset Alzheimer’s. So, stop sulking and be active!
Reference
- 2012. Early Onset Dementia: A national challenge and future crisis summary. Alzheimer’s Association. https://www.alz.org/national/documents/report_earlyonset_summary.pdf
- 2017. The genes associated with early-onset Alzheimer’s disease. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5871104/
- 2019. What Causes Alzheimer’s Disease. National Institue of Aging. https://www.nia.nih.gov/health/what-causes-alzheimers-diseas
- 2022. What Are the Signs of Alzheimer’s Disease. National Institue of Aging. https://www.nia.nih.gov/health/what-are-signs-alzheimers-disease
- 2021. Exercise in the early to middle stages of dementia. Alzheimer’s Society. https://www.alzheimers.org.uk/get-support/daily-living/exercise/early-middle-dementia#:~:text=Walking%2C%20gardening%20and%20housework%20are,continue%20these%20activities%20where%20possible.
Also Read
EFFECTIVE WAYS TO PREVENT ACNE FOR CLEAR SKIN IN ADULTS
MAGNESIUM DEFICIENCY SYMPTOMS AND PRACTICAL TIPS TO MANAGE IT
DISCOVERING 5 EFFECTIVE WAYS FOR PREVENTION OF ASTHMA
Recognizing The Silent GERD Symptoms Beyond Heartburn

Have you ever experienced an annoying sensation in your stomach? It feels like the acid in your stomach is bubbling toward your throat. If yes, you may have chronic heartburn. Sometimes, it’s normal to experience heartburn from eating greasy foods. Yet, many times, it could be something more severe.
GERD symptoms encompass a range of uncomfortable experiences. It includes heartburn, acid reflux, and difficulties with swallowing. These symptoms can impact the quality of life. Thus, you should never ignore it.
GERD stands for a medical condition called gastroesophageal reflux disease. This medical condition occurs when the acid in your stomach rises. It could be to your mouth, lungs, and esophagus.
The truth is the condition isn’t rare. Yes, you heard it right! According to studies, around 18 to 27% of people in North America suffer from the same. If you want to know “what are the symptoms of GERD”, keep reading this post. Read all about warning signs, indicators of GERD, risk factors, and treatments.
What Are the Gastroesophageal Reflux Disease Symptoms?
-
Bitter taste in the mouth
One of the first GERD symptoms is a bitter taste in your mouth. GERD moves the food and bile from your tummy into your throat. It might cause a bitter taste in your mouth. At the same time, you may also experience a burn in your esophagus. It is unpleasant and painful. It is one of the GERD symptoms when your throat feels hot and sore. Additionally, you also produce more saliva than usual. It almost feels as if your throat is on fire. So, if this happens to you, do not shrug it off as a one or two-time occurrence.
-
Consistent heartburn
Many people who experience heartburn think that the heartburn will go away. Usually, people prefer to take antacid. Yet, sometimes, it does not work. Remember that it might not be a simple heartburn when it does not go away. It could be a severe symptom that leads to a burning sensation in the chest. It is normal to feel regurgitation and heartburn at times. But if it happens often, you may have contracted GERD.
-
Difficulty swallowing
It is another GERD symptom if you experience a feeling of food getting stuck in your throat. It’s important to recognize the symptoms and address them. Make sure you’re getting proper diagnosis and appropriate management of GERD. When you have GERD, you feel like the food is getting stuck in your throat. This condition is dysphagia. Remember that this condition can make it difficult to swallow. It can also make you feel like you do not want to eat. The condition flares up when eating some specific food. For example, spicy foods, chocolate, acidic foods, soft cheeses, and caffeine.
-
You feel like a heart attack is on its way
Another one of GERD symptoms in adults is that you feel like you are experiencing a heart attack. Since the chest is next to the heart, you might mistake it for cardiac symptoms. This suggests you might consider you’re having a heart attack. Other than burning, you can also feel pain when suffering from GERD. That is another reason people think they are having a heart attack. Remember that if you are unsure what is causing your chest pain, the best option is to see a physician. You can find out the truth and get medications. You should never assume that you have GERD. Moreover, never head to the neighborhood pharmacy for over-the-counter medication.
-
You may suffer from a persistent cough
Stomach acid can travel up your food pipe, reaching your lungs. This leads to respiratory problems. They can be minor and give you a hoarse cough. It might cause congestion in your chest. Also, you may even suffer from a persistent cough. Sometimes, respiratory issues can cause pneumonia, wheezing, laryngitis, or asthma. This is why you should consider seeing a physician to determine the cause.
-
You may face respiratory problems
If you feel shortness of breath, it is one of the many GERD symptoms. GERD may cause some respiratory problems. It includes aspiration or bronchospasm. So, you should know that these conditions can become life-threatening. So, never ignore such symptoms.
Serious Issues That Could Happen If GERD Is Left Untreated
You need to remember that GERD symptoms and treatment go hand in hand. If left untreated, GERD can lead to more serious health conditions. Yes, that’s true!
- One condition is esophagitis. Esophagitis happens when acid damages the lining inside the esophagus.
- Other conditions that may occur from acid reflux disease include a hiatal hernia. Hiatal hernias form when the stomach slides into the chest from your diaphragm.
- GERD can also turn into esophageal ulcers or esophageal strictures. At worst, it could turn into a pre-cancerous condition called Barrett’s esophagus. It’s also known as esophageal cancer.
Risk factors
There are several risk factors for GERD. Here are some of them:
- Obesity and excess body weight can increase abdominal pressure. It can lead to a higher likelihood of acid reflux.
- A hiatal hernia can also contribute to GERD. It’s a condition where part of the stomach protrudes through the diaphragm.
- Other factors include smoking, which weakens the lower esophageal sphincter. It could be pregnancy, which places pressure on the abdomen. Then, there are certain medications like antihistamines and calcium channel blockers.
- Dietary choices can also exacerbate GERD symptoms. For instance, consuming fatty and spicy foods, alcohol, and caffeine.
These negative risk factors can contribute to the development of GERD symptoms. Manage these risks and make lifestyle changes to reduce their occurrence and severity.
Causes of GERD
Like any other disease, many factors can cause GERD. Here are some causes of GERD in adults.
- Weak lower esophageal sphincter (LES)
- Hiatal hernia
- Abnormal esophageal contractions
- Delayed stomach emptying (gastroparesis)
- Increased abdominal pressure
- Obesity and excess body weight
- Pregnancy
- Smoking
- Certain medications (e.g., antihistamines, calcium channel blockers)
- Dietary factors (e.g., fatty and spicy foods, citrus fruits, chocolate, caffeine)
- Alcohol consumption
- Stress and anxiety
These factors can contribute to the development of GERD. It might impair the function of the LES. It may increase acid production or disrupt the normal digestive process.
Hence, it’s important to identify and address these causes of GERD in older adults. This can manage the symptoms.
When to Contact Your Physician?
Contact your physician immediately if you’re experiencing any of the above-mentioned symptoms. No matter whether it’s shortness of breath, persistent cough or chest pain.
Your doctor will do some tests. In case you have GERD, they may prescribe what’s known as a proton pump inhibitor for treatment. Some of the medications may include but are not limited to:
- Omeprazole
- Esomeprazole
- Lansoprazole
The above are the most common medicines to treat GERD. But there are other medical options as well. Moreover, your physician may also refer you to a gastroenterologist for further testing.
Home Remedies to Treat GERD
You can take steps at home to relieve your GERD symptoms. Here are some of the things that can help.
- Eat three to four hours before bedtime. It’ll give your food time to digest while still awake.
- Elevate your head when you get ready for bed. You can prop your pillows up high.
- Sleep on your left side to avoid irritation due to the shape of the stomach.
Following these tips will help relieve your GERD. Plus, it’ll allow you to sleep more well through the night.
Final Words
We hope that you know the symptoms of gastroesophageal reflux disease. You might experience these when you have GERD. Yet, this condition can cure with medication, proper diet, and sleep adjustments. You should immediately visit your doctor if you experience any of these symptoms. If you already have a prescription from your doctor, contact our pharmacy. We offer affordable medications and help you save on various prescriptions.
References
- 2002. Joel J. Heidelbaugh. Gastroesophageal Reflux Disease (GERD). Michigan Medicine. https://www.med.umich.edu/1info/FHP/practiceguides/gerd/gerd.12.pdf
- 2013. National Institute of Diabetes and Digestive and Kidney Diseases. San Francisco Surgical. Gastroesophageal Reflux (GER) and Gastroesophageal Reflux Disease (GERD) in adults. https://sfsurgery.com/wp-content/uploads/2014/06/Gastroesophageal-Reflux-Disease-GERD.pdf
- 2019. J. family Med Prim Care. Prevalence and risk factors of gastroesophageal reflux disease. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6436310/
- 2021. Anna Taraszewska. Risk Factors for Gastroesophageal Reflux Disease Symptoms Related to Lifestyle and Diet. National Institute of Public Health. https://wydawnictwa.pzh.gov.pl/roczniki_pzh/media/Taraszewska_RPZH_2021_Vol%2072.pdf
- 2021. Rasool MF. Assessing the Frequency and Risk Factors Associated with Gastroesophageal Reflux Disease (GERD). Dove Press. https://www.dovepress.com/assessing-the-frequency-and-risk-factors-associated-with-gastroesophag-peer-reviewed-fulltext-article-RMHP
Also Read
10 FOODS THAT REDUCE ANXIETY AND THE ONES THAT WORSEN IT
UNCOVERING TOP 6 EXPERT TIPS FOR A HEALTHY HEART
Understanding Endometrial Cancer Treatment and Diagnosis

In the realm of women’s health, the battle against cancer stands as one of the greatest challenges. Among the various forms of this relentless disease, endometrial cancer emerges as a prominent adversary.
So, with a mission to empower and enlighten, this blog will unravel the mysteries surrounding this prevalent gynecological cancer, shedding light on endometrial cancer treatment, risk factors, and diagnosis.
What increases the Endometrial Cancer Risk Factors?
These are some factors that may increase the risk of endometrial cancer:
- Early menstruation (starting before age 12)
- Early menopause (before age 50)
- Endometrial polyps
- Estrogen replacement therapy
- Irregular periods
- Never being pregnant
- Obesity
- Polycystic ovary syndrome (PCOS)
- Tamoxifen use (a drug for breast cancer treatment)
Endometrial Cancer Prognosis
Endometrial cancer prognosis is a crucial aspect of understanding the potential outcome and future course of the disease. Factors such as the stage of cancer at diagnosis, grade of the tumor, and the presence of specific biomarkers play significant roles in determining prognosis.
A favorable prognosis is often associated with early-stage diagnosis, lower tumor grade, and the absence of metastasis. However, you should know that each case is unique, and the prognosis may vary. Through advanced medical advancements and personalized endometrial cancer treatment approaches, medical professionals strive to optimize outcomes and provide hope to individuals facing endometrial cancer.
Aside from these factors, some health conditions also increase the risk of developing cancer, and these conditions include breast cancer, colon cancer, diabetes, gallbladder disease, and high blood pressure.
Endometrial Cancer Diagnosis
This condition is usually detected at very early stages because it produces abnormal vaginal bleeding. This symptom urges women to see their doctors. When the condition is diagnosed early on, surgery can be performed to remove the uterus, which successfully cures the condition. Other signs and symptoms of endometrial cancer include:
- Abnormal blood-tinged discharge from the vagina
- Bleeding in between periods
- Pain during intercourse
- Pain in the pelvis
- Vaginal bleeding after menopause
Seeing a doctor and seeking endometrial cancer treatment right away is important whenever you experience any of these symptoms. While they may be signs of a completely different condition, it’s still essential to get checked right away to ensure that the condition is ruled out.
What Are Some Endometrial Cancer Treatment Methods?
1. Surgery
Surgery is done to remove the uterus, and oftentimes, the fallopian tubes and ovaries, too. This is believed to be a major alternative treatment for endometrial cancer. It is usually done for the early stages of cancer when the problem is still contained inside the uterus.
2. Radiation Treatment
Radiation treatment for endometrial cancer is yet another way to combat this cancer. This endometrial cancer treatment method makes use of powerful energy beams to kill cancer cells. In some cases, radiation may also be done prior to doing surgery, as it shrinks tumors and makes them easier to remove.
3. Hormone therapy
Another effective method to fight this cancer is hormone treatment for endometrial cancer. It involves the intake of medication, which in turn affects the hormone levels in the body. This is usually done for those with advanced endometrial cancer, especially that which has already spread outside the uterus.
4. Chemotherapy
One of the most common cancer treatments, chemotherapy uses chemicals to kill cancer cells and is also recommended for women with advanced levels of endometrial cancer. So, we can say that chemotherapy is an effective metastatic endometrial cancer treatment.
Endometrial Cancer Staging
If indeed you are diagnosed with endometrial cancer, you will need to undergo endometrial cancer staging treatment. Your treatment method will depend on the various characteristics of the disease. Some of them are what stage it is, your overall health, and of course, your preferences in terms of treating it.
Final Thoughts
Endometrial cancer, just like other diseases, should not be ignored as it can prove to be fatal. Now that you know about its risk factors, make sure to take precautions. And if you notice any of the above mentioned symptoms, contact a doctor immediately for diagnosis. Remember that only effective endometrial cancer treatment can help you fight that dangerous disease.
Also Read
UNVEILING THE DANGEROUS ASPARTAME SIDE EFFECTS ON HEALTH
SLEEP APNEA: THE SURPRISING CULPRIT BEHIND YOUR RESTLESS NIGHTS
TIPS TO MAINTAIN AN ACTIVE LIFESTYLE WITH EARLY ONSET ALZHEIMER’S
Understanding How to Lower Triglycerides Naturally?

Recent studies have shown that borderline patients with high levels of triglyceride can lower triglycerides with a change in lifestyle and a change in diet. Yes, you heard it right!
Triglycerides are a form of fat in the bloodstream that can rise if someone is overweight, inactive, a smoker, consumes too much alcohol or eats a diet high in carbohydrates. Are you wondering why and how to lower triglycerides naturally? Well, lowering triglycerides naturally can help reduce the risk of heart disease and improve overall health. And as for how to lower it, keep reading as we are going to tell you about the best way to lower triglycerides.
Understanding the Levels of Triglycerides
What is a normal triglyceride number and how to lower triglycerides? Now that you know what are, let us understand this as well. Experts from a screening study demonstrated that people who have less than 100mg/dL of triglycerides are the healthiest and that these levels are optimal. Remember that the normal triglyceride level for males and females might differ a bit.
Borderline triglyceride patients have levels between 150-199mg/dL. Remember that borderline patients should consider losing 5% of their body weight and limiting their calorie intake along with limiting sugars to less than 10% of their total intake. You should know that weight loss has shown valuable changes in lipids and lipoproteins. So, with a 5-10% loss of body weight comes positive benefits such as a 20% reduction of triglycerides, a 15% decrease in LDL cholesterol, and an 8-10% decrease in HDL cholesterol.
2 Ways to lower triglycerides
Now, get ready to know how to lower triglycerides naturally as we are about to tell you how to quickly lower triglycerides.
Triglycerides diet
There has been a lot of confusion about the best way to lower triglycerides and how much it actually affects the cardiovascular system. Borderline patients are recommended to consume no more than 100g of fructose from processed foods. Foods that assist in triglyceride treatment include fruits and vegetables that are low in fructose, such as strawberries, grapefruit, bananas, and peaches should be eaten. A diet to lower high TGL causes should consist of high-fiber whole grains and healthy unsaturated fats such as omega-3 fatty acids along with high triglyceride meds.
Triglycerides and exercise
Remember that you should do exercise to lower triglycerides. We are saying this because regular exercise can help lower triglycerides by increasing muscle mass, improving insulin sensitivity, reducing body fat, and making sure that you have only good triglycerides. If we talk about the duration of exercise, at least 150 minutes per week should help reduce triglycerides.
Conclusion
So, if you didn’t know how to lower triglycerides naturally, we hope that now you are familiar with everything about it. And we believe that when you know how to reduce high triglyceride symptoms, all you need to do is manage your diet and exercise.
Also Read
7 GAME-CHANGING TIPS FOR MANAGING TYPE 2 DIABETES
EXPLORING THE INTRICATE LINK BETWEEN CORTISOL AND SLEEP PATTERNS
DISCOVERING 5 EFFECTIVE WAYS FOR PREVENTION OF ASTHMA
Discovering Impactful Ways for Type 2 Diabetes Management

We know that finding out that you have type 2 diabetes can come as a shock. But, once you know it, you need to find ways for type 2 diabetes management. It’s true that you’re going to need to make some major adjustments to your daily routine. But with the right plan to manage type 2 diabetes, you don’t have to let it ruin your life.
Developing a care plan after being diagnosed with type 2 diabetes will help you manage your diabetes and take back control over your life. Wondering how to do it? Well, continue reading to find out how you can live happily with a Type 2 Diabetes management plan.
1. Make A Type 2 Diabetes-friendly Diet Plan
If you want to maintain your blood sugar levels, you’re going to need a good diet plan. Remember that you can make your daily routine a lot easier by planning your meals ahead of time.
Stock up on healthy and nutritious meals that can be made quickly and help you in type 2 diabetes management. Start by buying whole foods such as fruits and vegetables. For protein, you should stick to organic, lean meats such as chicken, turkey, and fish.
You can also find plant-based protein sources such as spinach, quinoa, and legumes. But when you are choosing plant-based proteins, be sure to limit the number of carbohydrates you eat. On average, you should get 45-60% of your daily calories from carbs as someone who is looking forward to managing type 2 diabetes.
Getting into a comfortable routine and planning will help you stick to a type 2 diabetes diet plan and avoid dangerous spikes in your blood sugar levels. You should also get in the habit of checking food labels and looking for nutritional facts about the foods you eat to be informed. You can consult with a nutritionist to help you get on track and help you eat a well-rounded diet.
2. Watch Your Carbs Intake
Since carbohydrates turn to sugar in your body, it’s no wonder that watching your carbs is a big part of how to work on type 2 diabetes management. You should know that having type 1 or 2 diabetes means that your body has a difficult time processing and using blood sugar.
Your body needs carbs to function but not all carbs are created equally. Remember that eating complex carbs and fiber is much better for you because they take longer to break down during digestion. This further means that you won’t experience a giant spike in your blood sugar.
There are three main types of carbohydrates: starches, sugars, and fiber. Starches are complex carbs such as potatoes, beans, and grains like brown rice or quinoa. Sugars are both naturally occurring in fruits or added in sweets like chocolate or yogurt. Fiber, on the other hand, is commonly found in vegetables such as green beans and broccoli. It is also found in eggs, meat or fish.
You need to keep in mind that complex carbs such as starches and fiber that are naturally occurring are a safer bet for type 2 diabetes management. This is because your body slowly breaks them down.
Added sugars should be avoided (or eliminated) as much as possible since it causes your insulin levels to spike quicker. Tracking your carbs every day will help you to avoid having too much sugar. The best thing is that you can find tracking apps on your phones that make tracking food more convenient.
3. Do Regular Exercise
Another way for diabetes management type 2 is through regular fitness and exercise. It’s true that having a healthy diet can make a big difference but there’s no substitute for being active. Yes, you heard it right!
Doing exercise is not only going to help you get in shape and stay healthier, but it also makes you feel better. Find a regime that you enjoy and that works with your schedule. It can be as simple as taking a walk around your neighborhood or spending 30 minutes at the gym.
Remember that everyone’s fitness level is different, so you should consult with your doctor or trainer for a workout plan that is safe for you and helps in type 2 diabetes management. Have fun with your exercise and don’t be afraid to mix it up so that you don’t get bored. You can even listen to music or find a workout buddy to help you stay motivated as well.
4. Use Medication
Another key component to managing your type 2 diabetes effectively is taking your medication on time for diabetes type 2. Managing it can become much easier with the help of a doctor as they’ll prescribe the right medication. Your doctor may test your blood sugar two to four times a year using the A1C test. From there, you can discuss your personal goals and determine the proper medication, meal plan, and exercise level based on your age and other categories.
Remember that you might be required to test your blood sugar level regularly as part of your treatment plan. If you’re taking insulin medications, this might mean multiple tests throughout the day. Yes, that’s true.
Your doctor may combine different medications and insulin therapy depending on your personal circumstances and the other medications you are on. Remember that you can keep up with your medications by refilling prescriptions online.
Which Medication Is Right for You?
A common medication for type 2 diabetes management is metformin which is used to lower glucose production in your liver. It is usually the first medication prescribed to treat type 2 diabetes.
Sulfonylureas and Meglitinides are medications prescribed to help your pancreas produce more insulin. Some examples are glyburide, glipizide, and glimepiride. Other medications such as DPP-4 inhibitors help to reduce blood sugar levels without causing weight gain. But you should be aware of the fact that they have some side effects such as joint pain and risk of pancreatitis.
Injectable medications, such as GLP-1 receptor agonists, slow your digestion to help reduce blood sugar levels. These can also help with weight loss. Although they could cause nausea and increase your risk of pancreatitis.
SGLT2 inhibitors, on the other hand, prevent your kidneys from reabsorbing sugar by excreting it instead. This drug class can help to reduce your risk of heart attack and stroke. So, it is prescribed to people who are at high risk of these conditions.
A Look at Insulin Therapy
Type 2 diabetes management through insulin therapy has grown in popularity for type 2 diabetes patients because of its effectiveness. Insulin is administered through injections because normal digestion is not effective. You should know that your doctor may have you take different types of insulin throughout the day.
You may start by taking one long-acting shot at night. Typically, insulin glargine (Lantus) or insulin detemir (Levemir) is prescribed. Be sure to talk to your doctor about the effects of the medications and insulin you are taking to find the one that works the best for you.
How To Create a Plan to Manage Type 2 Diabetes?
To make a type 2 diabetes management plan that is effective, you must commit to a strategy that incorporates a healthy diet, exercise, and medication(s). Combined, these three aspects can give you the best chance of maintaining your blood sugar level goals.
So, if you are looking for more ways to stay healthy and avoid an insulin spike? Check out the informative articles here.
Also Read
7 GAME-CHANGING TIPS FOR MANAGING TYPE 2 DIABETES
UNVEILING THE SURPRISING COCONUT WATER BENEFITS ON HEALTH
UNCOVERING THE TRUTHS BEHIND COMMON HEALTH MYTHS
Unveiling The Dangerous Aspartame Side Effects on Health

Could there be a link between breast cancer and artificial sweeteners? Well, there is! For years, manufacturers and the FDA reassured the public that natural sweeteners were completely safe. But are they really? Today, let’s look at the relationship between breast cancer and artificial sweeteners, including how they work to cause cancer.
There are different types of artificial sweeteners out there like:
- Saccharin
- Sucralose
- Acesulfame potassium
For the sake of discussion, we are going to focus on the most popular sugar substitute type i.e., aspartame. So, keep reading if you want to know about the dangerous aspartame side effects, as we are going to talk about it in detail.
What is Aspartame?
Before we dive into the side effects of aspartame, let us first understand what it actually is. We can say that aspartame is a “first generation” sugar substitute. It’s 200 times sweeter than regular sugar, so it’s a favorite ingredient in many food and beverage products. We feel that some of you may know it as NutraSweet, Spoonful, and Equal.
At first, the FDA didn’t approve of this as a sugar substitute. But through dirty politics and regulatory tactics, G.D. Searle & Company finally got the go signal to sell it as an artificial sweetener in dry goods in 1981. And it is quite obvious that they didn’t care at all about the aspartame effects as all that mattered to them was profit and money.
We know that many of you might be wondering about whether aspartame is 100% safe or not, right?
How Does Aspartame Affect Your Health?
For decades, health advocates have been asking the FDA to re-evaluate their decision about artificial sweeteners because breast cancer is believed to be one of the most fatal possible aspartame side effects. Yes, that’s true.
Health groups aren’t really happy and want the FDA to re-evaluate their decision because one of the effects of aspartame is that it may play a role in the incidence of breast cancer. For instance, there are higher incidences of breast and prostate cancers in North America and Europe compared to Asia and Africa, which have lower consumption of NutraSweet, another brand name for non-nutritive sweeteners.
You should know that inside the body, aspartame is broken down into methanol (10 percent), aspartic acid (40 percent), and phenylalanine (50 percent). Experts say that these compounds are highly safe because fresh fruits and veggies have them.
You might be thinking about why we were talking about the side effects of aspartame then, right? Well, here’s where it gets ugly.
Once taken, the body converts aspartame into methanol within minutes. The next step is converting methanol into formaldehyde, a compound linked to cancer in humans. Yes, you heard it right! And in his study, Dr. Monte reaffirmed this fact and added that it’s not only the liver that metabolizes this compound.
Aside from the liver, one of the few richest sources of Alcohol Dehydrogenase Enzyme (ADH) in the body is human breasts, specifically the mammary endothelial cells. And you need to keep in mind that most cases of human breast cancer normally start in the mammary epithelial cells.
Aspartame Does More Harm Than Good
We agree that not everyone who uses artificial sweeteners is bound to get sick, but…
We can’t simply ignore population studies and clinical trials that suggest that artificial sweeteners, like aspartame, may contain certain ingredients that could put a person at risk for different types of illnesses, like diabetes and cancer. Yes, we cannot just ignore the studies that point to various aspartame side effects. The result of one animal study even suggests that exposure to aspartame in the womb could cause blood and breast cancers.
So, what are your thoughts on the issue of breast cancer linked to using aspartame?
Final Words
We hope that your question about “aspartame: good or bad” is answered now. It is obviously not good for our health. We believe that natural sweeteners, such as honey, maple syrup, and agave nectar, are great alternatives to artificial sweeteners. These sweeteners can be used in place of sugar in recipes and are often promoted as healthier options due to their lower glycemic index and potential health benefits.
Also Read
DISCOVER THE MIRACULOUS HEALTH BENEFITS OF POMEGRANATE
7 GAME-CHANGING TIPS FOR MANAGING TYPE 2 DIABETES
SLEEP APNEA: THE SURPRISING CULPRIT BEHIND YOUR RESTLESS NIGHTS
Unveiling The Secret Signs of ED To Fight It

Erectile dysfunction: two words you never want beside each other. When it’s mentioned we all become silent and get awkward, right? Well, of course, yes! The truth is that about 30 million Americans suffer from erectile dysfunction. Yes, you heard it right.
ED in men is a topic that we try to avoid even when talking about it to doctors. So, let’s talk about the causes and signs of ED and ways to treat it because what erectile dysfunction really means is in the back of every guy’s mind. Let’s get started, shall we?
What is Erectile Dysfunction?
In simple words, we can say that erectile dysfunction is impotence. If you are wondering about the primary sign of erectile dysfunction, remember that it is the failure to achieve or sustain an erection for satisfactory sexual intercourse. But try not to get confused with decreased libido and problems with orgasms and ejaculation because that is not part of erectile dysfunction.
If a man suffers from erectile dysfunction, the common reply is “don’t worry it’s all in your head, it will go away over time.” All you need to do is understand the causes and signs of erectile dysfunction. If you’re wondering what causes it, doctors would say if it were temporary then it’s a physiological issue. Yes, you heard it right! For an erection to occur it requires the interaction of your brain, nerves, hormones, and blood vessels.
Causes of Erectile Dysfunction
Now that you know about the meaning and signs of ED, let us have a look at the common causes of erectile dysfunction.
- diabetes
- high blood pressure
- poor blood flow
- depression neurological disorders
- sleeping pills,
- antidepressants,
- nerve damage,
- nicotine,
- alcohol,
- cocaine,
- stress,
- fear and bad communication between your partners.
How To Treat Erectile Dysfunction?
So, now that you know more about ED signs and what erectile dysfunction really is, the next step is figuring out what you can do about it.
1. See a doctor
When you notice the signs of ED, your first step to treat it should be to see a doctor and get an expert opinion. Generally, if you are facing erectile dysfunction then the best remedy that doctors generally suggest is to try and make some lifestyle changes first such as exercising more, having a better diet, and getting more sleep.
2. Understanding And Resolving the Mental Problems
It is important to explore the connection between mental health and erectile dysfunction so that you can manage both conditions. Then you should move on to tackle those mental problems that could be causing your dysfunction. And if you have a partner, it is a good idea to find better ways to communicate between the two of you.
3. Erectile Dysfunction Pills
Your next step, after noticing signs of ED, can be taking erectile dysfunction medication pills such as phosphodiesterase type 5 inhibitors like Viagra, Cialis, and Levitra or prostaglandin E1 analogs like Caverject and Muse. Remember that there are other ED medication treatment options available as well if taking pills isn’t your thing. For example, you could use a penile implant, vacuum pump devices, or go for surgery.
Conclusion
We know that the topic of erectile dysfunction is either on the down low or used as a joke, but the signs of ED in men should be taken seriously. If you suffer from this condition or notice signs of ED, remember that you are not alone and there’s no need to get stressed. Don’t let ED deter you; summon the courage to talk to your doctor and fight back to get rid of that problem.
Also Read
EXPLORING 5 PROVEN METHODS FOR NATURAL ED TREATMENT
MAGNESIUM DEFICIENCY SYMPTOMS AND PRACTICAL TIPS TO MANAGE IT
SLEEP APNEA: THE SURPRISING CULPRIT BEHIND YOUR RESTLESS NIGHTS