Why is Gemtesa So Expensive and How to Find Financial Relief

If you’ve been prescribed Gemtesa for overactive bladder, you may have experienced sticker shock at the pharmacy. With a list price of around $552 for a 30-day supply, Gemtesa ranks among the more expensive overactive bladder medications available today. For many Americans, especially those on fixed incomes, high Gemtesa costs can make treatment feel out of reach. But why is Gemtesa so expensive? And more importantly, what can you do to reduce these costs? This guide will help you understand the factors behind Gemtesa’s pricing and explore practical ways to make this medication more affordable.
What Is Gemtesa?
Gemtesa is the brand name for vibegron, a prescription medication used to treat overactive bladder (OAB) in adults. The FDA approved Gemtesa in December 2020, making it one of the newer options for managing OAB symptoms like frequent urination, urgency, and incontinence.
What makes Gemtesa different from other OAB medications is how it works. Vibegron belongs to a class of drugs called beta-3 adrenergic agonists. These medications target specific receptors in the bladder muscle, helping it relax and hold more urine. This mechanism is different from anticholinergic medications like oxybutynin, which can cause more side effects like dry mouth and constipation.
Approximately 33 million U.S. adults have overactive bladder, according to the Urology Care Foundation. This large patient population represents a significant market for pharmaceutical companies developing OAB treatments. Gemtesa was developed by Urovant Sciences and is now marketed by Sumitomo Pharma America.
The medication comes as a 75 mg tablet taken once daily with or without food. Clinical trials showed that Gemtesa can reduce the average number of daily bathroom trips and accidents in people with overactive bladder.
Factors Contributing to Gemtesa’s High Cost
Understanding why Gemtesa costs so much requires looking at the complex factors that influence drug pricing. Multiple elements contribute to the high price tag, from initial development costs to marketing expenses.
Research & Development Costs
The journey from laboratory to pharmacy shelf is long and expensive. On average, it costs between $1 billion and $2.8 billion to develop a new drug, according to research published in JAMA. This massive investment includes not just the successful drug, but also the many failed candidates that never make it to market.
For every drug that receives FDA approval, pharmaceutical companies typically test hundreds or thousands of potential compounds. Most of these fail at various stages of development. The companies must recoup these losses through the successful medications they bring to market.
Vibegron’s development took years of research to identify the compound, understand how it works, and optimize its formulation. Scientists had to prove it was both safe and effective before moving to human testing. All of this research requires significant financial investment in laboratories, equipment, and skilled researchers.
Clinical Trial Expenses
Before the FDA approves any new medication, it must undergo rigorous clinical testing. Gemtesa’s pivotal trial, called EMPOWUR, enrolled over 1,500 participants across multiple sites. Clinical trials of this size are extremely expensive to conduct.
The EMPOWUR trial was a Phase 3 study lasting 12 weeks, with participants randomly assigned to receive either Gemtesa or a placebo. Managing a trial of this scope requires hiring research coordinators, monitoring patient safety, collecting and analyzing data, and ensuring regulatory compliance.
Each participant in a clinical trial represents significant costs. The company must pay research sites, compensate participants for their time, and cover medical monitoring. When you multiply these costs across thousands of participants and multiple trial phases, the expenses add up quickly.
Patent Protection & Market Exclusivity
When a pharmaceutical company develops a new drug, they receive patent protection that prevents generic competition for a specific period. Brand-name drugs can have up to 20 years of patent exclusivity from the time they file their initial patent application.
Additionally, new chemical entities (NCEs) like vibegron receive 5 years of data exclusivity from the FDA. This means even if the patent expires, generic manufacturers cannot use the original company’s safety and effectiveness data to get their own approval for 5 years.
This exclusivity period allows companies to set higher prices without generic competition. Once patents expire and generics enter the market, prices typically drop significantly. However, Gemtesa is still relatively new, so generic versions are not yet available.
Marketing & Advertising Spending
Pharmaceutical companies spend billions on marketing their products to both healthcare providers and consumers. In 2022, U.S. direct-to-consumer pharmaceutical advertising totaled $8.07 billion, according to Statista.
You’ve likely seen Gemtesa advertisements on television or in magazines. These marketing campaigns are expensive to produce and air. The company also employs sales representatives who visit doctors’ offices to educate healthcare providers about the medication’s benefits.
Professional medical education, conference sponsorships, and clinical research presentations all represent additional marketing costs. While these activities can provide valuable medical education, they also contribute to the overall cost of bringing a medication to market.
Manufacturing & Quality Control
Producing pharmaceutical-grade medications requires specialized facilities that meet strict FDA standards. These manufacturing plants must maintain precise environmental controls, use high-quality raw materials, and follow detailed quality control procedures.
Every batch of Gemtesa must undergo extensive testing before release to ensure it meets specifications for potency, purity, and safety. This quality control process requires sophisticated laboratory equipment and trained personnel.
The manufacturing facilities themselves represent significant capital investments. Companies must build or lease specialized production lines, install monitoring systems, and maintain backup capabilities to ensure consistent supply.
Regulatory Approval Process
Getting FDA approval involves substantial fees and administrative costs. The FDA charges user fees for new drug applications, which can exceed $3 million for a standard application. These fees help fund the FDA’s review process but add to the overall development costs.
Beyond the initial approval, companies must continue to pay annual fees to maintain their drug’s approval status. They must also fund post-market safety monitoring and submit regular safety reports to the FDA.
Regulatory compliance requires dedicated staff to manage FDA communications, maintain required documentation, and ensure ongoing adherence to safety regulations. These operational costs continue throughout the product’s lifecycle.
PBM & Insurance Negotiations
The drug pricing landscape involves complex negotiations between pharmaceutical companies and pharmacy benefit managers (PBMs). These middlemen manage prescription benefits for insurance companies and negotiate rebates with drug manufacturers.
While the list price (called the Wholesale Acquisition Cost or WAC) for Gemtesa might be $552, the actual amount paid often differs significantly due to rebates and discounts negotiated behind closed doors. However, patients often pay based on the list price, not the discounted net price.
This system can result in patients paying more out-of-pocket while insurance companies and PBMs receive substantial rebates. The complexity of this system contributes to the disconnect between list prices and actual treatment costs.
Perceived Innovation & Value
As a newer medication with a different mechanism of action, Gemtesa is positioned as an innovative treatment option. The beta-3 agonist class may cause fewer anticholinergic side effects compared to older OAB medications.
This perceived advantage allows the manufacturer to command premium pricing. Healthcare providers and patients may be willing to pay more for a medication that offers improved tolerability or effectiveness compared to existing options.
The value proposition extends beyond just treating symptoms to potentially improving quality of life with fewer bothersome side effects. This positioning supports higher pricing in the marketplace.
How Gemtesa’s List Price Is Determined
Understanding how pharmaceutical companies set prices requires distinguishing between different pricing concepts and how they affect what patients actually pay.
Wholesale Acquisition Cost vs. Net Price
The Wholesale Acquisition Cost (WAC) represents the list price that pharmacies pay to acquire medications from manufacturers. For Gemtesa 75 mg (30 tablets), the WAC is approximately $552. This is the “sticker price” you’ll often see quoted.
However, the net price – what’s actually paid after rebates and discounts – is typically much lower. Insurance companies and PBMs negotiate substantial rebates that can reduce the effective price by 20-50% or more. Unfortunately, patients rarely benefit directly from these hidden discounts.
The WAC serves as the starting point for most pricing calculations, including insurance copays and deductibles. This means patients often pay based on the higher list price, even though the actual transaction price is lower.
Insurance Coverage & Out-of-Pocket Costs
Most insurance plans cover Gemtesa, but your out-of-pocket costs depend on your specific plan details. If you have a copay-based plan, you might pay a fixed amount like $30-50 per month. With coinsurance, you pay a percentage of the drug’s cost, perhaps 20-30%.
High-deductible health plans require you to pay the full price until you meet your annual deductible. This can mean paying the entire $552 monthly cost early in the year, which creates a significant financial burden for many patients.
Your plan’s formulary (list of covered medications) also affects costs. If Gemtesa is on a higher tier, your copay will be larger. Some plans may not cover it at all without prior authorization.
Medicare & Medicaid Coverage
Medicare Part D coverage for Gemtesa varies by plan. Most plans include it on their formularies, but it’s typically placed on higher tiers with larger copays. During the coverage gap (donut hole), you may pay up to 25% of the drug’s cost.
Medicare patients might face prior authorization requirements, meaning your doctor must prove medical necessity before coverage begins. This process can delay treatment and create additional administrative burden.
Medicaid coverage differs by state, but most state programs cover Gemtesa with prior authorization. The approval process typically requires trying and failing other, less expensive OAB medications first.
Prior Authorization & Step Therapy
Many insurance plans require prior authorization for Gemtesa, meaning your doctor must submit paperwork justifying the prescription before coverage begins. This process can take several days to weeks.
Step therapy requirements mandate trying less expensive alternatives first. You might need to fail treatment with generic medications like oxybutynin or tolterodine before insurance will cover Gemtesa.
These administrative hurdles are designed to control costs by steering patients toward less expensive options. While this can delay access to preferred treatments, understanding these requirements helps you and your doctor navigate the approval process more effectively.
Gemtesa vs. Other OAB Medications
Comparing Gemtesa to other overactive bladder treatments helps put its cost in perspective and may reveal more affordable alternatives.
Gemtesa vs. Myrbetriq
Myrbetriq (mirabegron) is another beta-3 agonist that works similarly to Gemtesa. Both medications target the same receptors and have comparable effectiveness for OAB symptoms.
Myrbetriq has been available since 2012 and costs approximately $400-450 for a 30-day supply – somewhat less than Gemtesa but still expensive. Generic mirabegron became available in 2023, offering a more affordable alternative with prices around $100-200 per month.
The choice between these medications often comes down to individual response and side effect profiles. Some patients tolerate one better than the other, making the higher cost worthwhile if it provides better symptom control.
Brand-Name vs. Generic OAB Drugs
Generic OAB medications cost significantly less than brand-name options. Generic oxybutynin, for example, costs $10-30 per month compared to hundreds for newer branded medications.
The trade-off is that older generic medications often cause more side effects. Anticholinergics like oxybutynin can cause dry mouth, constipation, and cognitive effects that may be particularly problematic for older adults.
Newer medications like Gemtesa were developed specifically to avoid these side effects, which justifies some of the price difference. However, not everyone experiences troublesome side effects with generic options, making them worth trying first.
Non-Drug Alternatives
Behavioral therapies and lifestyle modifications can effectively manage OAB symptoms without medication costs. Pelvic floor exercises, bladder training, and dietary changes may reduce symptoms significantly.
Physical therapy specifically focused on pelvic floor dysfunction can be highly effective. While this involves upfront costs, it may provide long-term symptom relief without ongoing medication expenses.
Combining behavioral approaches with less expensive medications often provides good results at lower overall costs. Your healthcare provider can help develop a comprehensive treatment plan that balances effectiveness with affordability.
Ways to Reduce Gemtesa Costs
Several strategies can help make Gemtesa more affordable, from manufacturer programs to insurance optimization.
Gemtesa Go Savings Program
Urovant Sciences offers the Gemtesa Go savings program for eligible patients. With this co-pay card, commercially insured patients may pay as little as $10 per month for their prescription. The program has income restrictions and doesn’t cover patients with government insurance like Medicare or Medicaid. You must have commercial insurance and meet other eligibility criteria to qualify. To enroll, visit the manufacturer’s website or ask your pharmacist about the program. The savings card can be used at most pharmacies and significantly reduces your monthly out-of-pocket costs.
Prescription Discount Cards
Services like GoodRx, SingleCare, and Optum Perks offer discount cards that can reduce Gemtesa’s cost even without insurance. These programs negotiate discounted rates with pharmacies and pass some savings to consumers. GoodRx, for example, might offer Gemtesa for $400-450 instead of the full $552 list price. While this is still expensive, it represents meaningful savings for uninsured patients or those with high deductibles. These discount programs are free to use and don’t require enrollment or income verification. Simply present the discount card or app at the pharmacy to receive the negotiated price.
Patient Assistance Programs
Several organizations offer patient assistance programs for those who cannot afford their medications. NeedyMeds maintains a comprehensive database of available programs and eligibility requirements. The Medicine Assistance Tool from the Partnership for Prescription Assistance helps patients find programs that match their specific situations. These programs may provide free or reduced-cost medications to qualifying individuals. Income limits vary by program, but many are designed to help middle-income patients who don’t qualify for Medicaid but still struggle with medication costs. Applications typically require documentation of income and insurance status.
Mail-Order & 90-Day Supply
Many insurance plans offer lower per-pill costs when you order 90-day supplies through mail-order pharmacies. This can reduce your effective monthly cost and minimize trips to the pharmacy.
A 90-day supply might cost $150 instead of $50 for three separate 30-day fills, creating modest but meaningful savings. Check with your insurance plan to see if this option is available.
Mail-order pharmacies also often provide better customer service for managing prior authorizations and insurance issues. They have dedicated teams to handle these administrative challenges.
Insurance Appeals & Formulary Exceptions
If your insurance doesn’t cover Gemtesa or places it on a high-cost tier, you can appeal this decision. Your doctor can request a formulary exception based on medical necessity. The appeals process requires documentation of why Gemtesa is medically necessary compared to covered alternatives. This might include failed trials of other medications or specific side effect concerns. While appeals take time and effort, they’re often successful when properly documented. Your doctor’s office may have staff experienced in managing these requests.
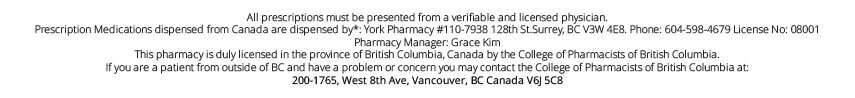
Canadian Online Pharmacies like PrescriptionPoint
For Americans facing high out-of-pocket costs for Gemtesa, licensed Canadian online pharmacies such as PrescriptionPoint.com offer a reliable, lower-cost alternative. By sourcing medications from Canada and overseas with regulated drug pricing, PrescriptionPoint helps U.S. customers access the same prescription drugs—often at significantly reduced prices. This is especially helpful for those without insurance or with high-deductible plans. Ordering through a trusted Canadian pharmacy can be a safe and affordable option to manage ongoing medication expenses.
Frequently Asked Questions
Is Gemtesa covered by Medicare?
Most Medicare Part D plans cover Gemtesa, but it’s typically placed on higher tiers with larger copays. You may need prior authorization, and during the coverage gap, you’ll pay a percentage of the drug’s cost. Check your specific plan’s formulary to understand your coverage details.
How much is a 30-day supply of Gemtesa?
The list price for a 30-day supply of Gemtesa 75 mg is approximately $552. However, your actual cost depends on insurance coverage, available discounts, and manufacturer programs. With the Gemtesa Go program, eligible patients may pay as little as $10 per month.
When will Gemtesa be available as a generic?
Generic versions of Gemtesa are not expected to be available for several years due to patent protection and data exclusivity. The medication received FDA approval in 2020, and new chemical entities typically receive 5 years of data exclusivity plus additional patent protection.
Is Gemtesa worth the money?
This depends on your individual situation and response to treatment. If you’ve tried less expensive alternatives without success or experienced intolerable side effects, Gemtesa’s higher cost may be justified. Discuss the cost-benefit analysis with your healthcare provider.
How can I get Gemtesa cheaper?
Several options can reduce costs: the manufacturer’s Gemtesa Go savings program, prescription discount cards like GoodRx, patient assistance programs, 90-day supplies, insurance appeals and Canadian online pharmacies like PrescriptionPoint.com. Start with the manufacturer program if you have commercial insurance, as this often provides the greatest savings.
Next Steps
If you’re struggling with Gemtesa’s cost, don’t give up on treatment. Start by discussing your financial concerns with your healthcare provider. They may be able to help you access manufacturer programs, apply for patient assistance, or find alternative treatments that fit your budget.
Contact your pharmacist as well – they often have extensive knowledge about available discount programs and can help you navigate different options. Many pharmacies also offer their own discount programs or can direct you to helpful resources.
Check with your insurance company about formulary exceptions or appeals processes. Sometimes a simple phone call can clarify coverage options or identify steps to improve your benefits.
Remember that managing overactive bladder effectively improves your quality of life significantly. While the costs can be challenging, various programs and strategies can make treatment more affordable. The key is exploring all available options and working with your healthcare team to find a solution that works for both your symptoms and your budget.
Another option worth exploring is PrescriptionPoint.com, an affordable destination for Gemtesa and other prescription medications. We offer competitive pricing and provide additional savings opportunities beyond traditional U.S. pharmacies. You can check our current gemtesa price in canada to compare costs and see if this option works for your situation.
With persistence and the right approach, you can find ways to make Gemtesa more affordable while effectively managing your overactive bladder symptoms.
References
- FDA.gov. (2024). Gemtesa Prescribing Information
- FDA.gov. (2020). Drug Trials Snapshot: GEMTESA
- Urologyhealth.org. (2024). What is Overactive Bladder (OAB)?
- Jamanetwork.com. (2016). Fewer Opioids, More Exercise for Severe Joint Pain From Arthritis
- Clinicaltrials.gov. (2021). A Study to Examine the Safety and Efficacy of a New Drug in Patients With Symptoms of Overactive Bladder (OAB) (Empowur)
- FDA.gov. (2020). Frequently Asked Questions on Patents and Exclusivity
- Drugs.com. (2025). Prices, Coupons, Copay Cards & Patient Assistance
- FDA.gov. (2017). Myrbetriq Prescribing Information
- Drugs.com. (2025). Generic Myrbetriq Availability
- Gemtesa.com. (2025). SIGN UP FOR INFO ON SAVINGS AND GEMTESA