Blood thinners have become essential medications for millions of Americans, with approximately 6 million people living with atrial fibrillation (AFib) – a number projected to reach 12.1 million by 2030 according to the CDC. Additionally, up to 900,000 U.S. cases of deep vein thrombosis (DVT) and pulmonary embolism (PE) occur annually, resulting in 60,000–100,000 deaths. While Eliquis has emerged as a leading anticoagulant, generating $12.2 billion in revenue for Bristol-Meyers Squibb in 2023, its high cost leaves many patients searching for affordable alternatives.
For seniors on fixed incomes, uninsured adults, and those exploring cross-border pharmacy options, understanding Eliquis alternatives becomes crucial for maintaining both health and financial stability. This comprehensive guide examines FDA-approved alternatives, their costs, safety profiles, and practical switching strategies.
What Is Eliquis?
Eliquis (apixaban) is a direct oral anticoagulant (DOAC) that belongs to a class of medications called Factor Xa inhibitors. Unlike traditional blood thinners like warfarin, which work through the vitamin K pathway, apixaban directly blocks Factor Xa, a key enzyme in the blood clotting cascade. This targeted mechanism helps prevent dangerous blood clots while potentially reducing bleeding risks compared to older anticoagulants.
The FDA has approved Eliquis for several critical indications. In patients with non-valvular atrial fibrillation, it reduces the risk of stroke and systemic embolism. For those who have experienced deep vein thrombosis or pulmonary embolism, Eliquis helps prevent recurrence. The medication is also approved for preventing DVT and PE in patients undergoing hip or knee replacement surgery.
Eliquis works by inhibiting both free and clot-bound Factor Xa, effectively interrupting the coagulation cascade at a crucial step. This mechanism allows for predictable anticoagulation without the need for routine blood monitoring, unlike warfarin which requires regular INR testing. The medication reaches peak blood levels within 3-4 hours and has a half-life of approximately 12 hours, necessitating twice-daily dosing.
Why Consider Alternatives?
Several compelling reasons drive patients to explore eliquis alternatives beyond the brand-name medication. Cost represents the primary concern for many Americans, particularly those without comprehensive insurance coverage. A 30-day supply of Eliquis 5 mg tablets costs between $787 at retail pharmacies, compared to generic warfarin at approximately $4 for the same period.
Bleeding complications, while less common with Eliquis than warfarin, still occur and may prompt physicians to consider alternative anticoagulation strategies. Some patients experience gastrointestinal bleeding, nosebleeds, or excessive bruising that interferes with their quality of life. Additionally, the twice-daily dosing requirement may pose challenges for patients with memory issues or complex medication regimens.
Insurance coverage limitations often force patients to explore different options. Some health plans may not cover Eliquis or may require substantial co-payments, making generic apixaban or other alternatives more financially viable. Prior authorization requirements can also delay treatment initiation, prompting consideration of immediately available alternatives.
Drug interactions and contraindications may necessitate switching to different anticoagulants. Patients taking certain medications that significantly interact with Eliquis, or those with specific medical conditions, may benefit from alternative blood thinners with different interaction profiles or monitoring requirements.
FDA-Approved Eliquis Alternatives
Generic Eliquis (Apixaban) – Bioequivalent Cost Savings
The FDA approved the first generic versions of apixaban on December 23, 2019, marking a significant milestone for cost-conscious patients. Generic apixaban contains the same active ingredient as brand-name Eliquis and must demonstrate bioequivalence, meaning it delivers the same amount of medication to the bloodstream at the same rate as the original.
Multiple manufacturers now produce generic apixaban, including Mylan, Teva, and Aurobindo Pharma. This competition has driven prices down considerably, with generic apixaban typically costing 60-80% less than brand-name Eliquis. Patients can expect to pay $100-$200 for a 30-day supply of generic apixaban, compared to $550-$600 for Eliquis.
The therapeutic equivalence of generic apixaban to Eliquis means patients can expect identical efficacy and safety profiles. The same dosing recommendations apply: 5 mg twice daily for most AFib patients, with dose reductions to 2.5 mg twice daily for patients meeting specific criteria including age ≥80 years, body weight ≤60 kg, or serum creatinine ≥1.5 mg/dL.
Rivaroxaban (Xarelto) – Once-Daily Convenience
Rivaroxaban, marketed as Xarelto by Bayer and Janssen, offers the convenience of once-daily dosing for most indications. Like Eliquis, Xarelto is a Factor Xa inhibitor that doesn’t require routine blood monitoring. The once-daily dosing may improve medication adherence, particularly important given that up to 25% of patients discontinue DOACs within the first year of treatment.
For atrial fibrillation, the standard Xarelto dose is 20 mg once daily with the evening meal. Patients with moderate kidney impairment (creatinine clearance 15-50 mL/min) receive a reduced dose of 15 mg daily. For DVT/PE treatment, patients typically start with 15 mg twice daily for 21 days, then continue with 20 mg once daily.
Cost-wise, Xarelto carries a similar price point to brand-name Eliquis, with 30-day supplies ranging from $500-$550. However, Bayer offers patient assistance programs and co-pay cards that can significantly reduce out-of-pocket costs for eligible patients. The convenience of once-daily dosing may justify the cost for patients who struggle with twice-daily regimens.
Dabigatran (Pradaxa) – Direct Thrombin Inhibition
Pradaxa (dabigatran) takes a different mechanistic approach as a direct thrombin inhibitor rather than a Factor Xa inhibitor. Manufactured by Boehringer Ingelheim, dabigatran directly binds to thrombin, preventing the conversion of fibrinogen to fibrin and subsequent clot formation.
The standard dose for AFib patients is 150 mg twice daily, with a reduced dose of 75 mg twice daily for patients with severe kidney impairment (creatinine clearance 15-30 mL/min). Pradaxa must be taken with a full glass of water and should not be crushed or opened, as this significantly increases bleeding risk.
A unique advantage of dabigatran is the availability of idarucizumab (Praxbind), a specific reversal agent that can rapidly neutralize dabigatran’s anticoagulant effects in emergency situations. This makes Pradaxa particularly attractive for patients at higher bleeding risk or those requiring urgent surgical procedures.
Pradaxa costs approximately $500-$530 for a 30-day supply, similar to other brand-name DOACs. The manufacturer provides patient assistance programs and co-pay cards to help reduce costs for eligible patients.
Edoxaban (Savaysa) – Simplified Dosing
Edoxaban, marketed as Savaysa by Daiichi Sankyo, represents another once-daily Factor Xa inhibitor option. The medication offers simplified dosing with fewer drug interactions compared to some alternatives, making it suitable for patients taking multiple medications.
For AFib patients, the standard dose is 60 mg once daily, reduced to 30 mg daily for patients with creatinine clearance 15-50 mL/min, body weight ≤60 kg, or concurrent use of certain P-glycoprotein inhibitors. Unlike some other DOACs, edoxaban should not be used in AFib patients with creatinine clearance >95 mL/min due to reduced efficacy.
Savaysa generally costs $480-$520 for a 30-day supply, positioning it competitively among DOAC options. The manufacturer offers patient support programs including co-pay assistance for commercially insured patients.
An important consideration with edoxaban is its metabolism through the liver. Patients with severe liver impairment should avoid this medication, and those with moderate liver disease require careful monitoring.
Warfarin (Coumadin/Jantoven) – Time-Tested Affordability
Warfarin remains the most cost-effective oral anticoagulant, with generic versions costing approximately $4 for a 30-day supply. As a vitamin K antagonist, warfarin has over 60 years of clinical experience and extensive research supporting its use across various patient populations.
The primary drawback of warfarin is the need for regular INR monitoring to maintain therapeutic anticoagulation levels between 2.0-3.0 for most indications. Patients typically require INR checks every 2-4 weeks once stable, with more frequent monitoring during initiation or dose adjustments.
Warfarin interacts with numerous medications and foods containing vitamin K, requiring patients to maintain consistent dietary habits and careful medication management. Despite these challenges, warfarin remains highly effective for stroke prevention in AFib and treatment of venous thromboembolism.
For patients who can successfully manage INR monitoring and dietary considerations, warfarin offers excellent anticoagulation at a fraction of the cost of newer agents. Many patients achieve stable INR levels and experience good quality of life on warfarin therapy.
Injectable Anticoagulants (Heparin, Enoxaparin) – Hospital and Transitional Use
Injectable anticoagulants like unfractionated heparin and low molecular weight heparins (such as enoxaparin/Lovenox) primarily serve specific clinical situations rather than long-term outpatient therapy. These medications are commonly used in hospital settings, for bridging therapy during warfarin initiation, or in patients who cannot take oral anticoagulants.
Unfractionated heparin requires continuous intravenous infusion with frequent monitoring of activated partial thromboplastin time (aPTT) levels. Enoxaparin can be administered subcutaneously once or twice daily and typically doesn’t require routine monitoring in patients with normal kidney function.
While these injectable options are not practical for most long-term anticoagulation needs, they play important roles in specific clinical scenarios and may be used temporarily while transitioning between oral anticoagulants.
Side Effects & Safety Profiles
Bleeding Risk Comparison – Clinical Trial Evidence
The landmark ARISTOTLE trial provided crucial safety data comparing apixaban to warfarin in AFib patients. Apixaban has demonstrated reduced bleeding risk compared to warfarin in clinical trials, but specific ARISTOTLE trial data is not available here for verification
Comparing bleeding rates across DOACs reveals important differences. Dabigatran shows higher gastrointestinal (GI) bleeding rates than warfarin, but direct comparisons of major bleeding rates across DOACs are not confirmed.
Gastrointestinal bleeding patterns differ among anticoagulants. Dabigatran shows higher rates of GI bleeding compared to warfarin, while apixaban demonstrates lower rates. Rivaroxaban and edoxaban show intermediate GI bleeding risks. These differences may influence anticoagulant selection for patients with prior GI bleeding history.
Other Common Adverse Effects
Beyond bleeding complications, anticoagulants can cause various other side effects that impact patient quality of life. Bruising represents the most commonly reported non-major bleeding symptom. While usually not medically significant, excessive bruising can cause cosmetic concerns and anxiety.
Dabigatran commonly causes GI symptoms, potentially due to its tartaric acid content. It particularly shows higher rates of dyspepsia, likely related to its tartaric acid formulation. Taking medications with food can help reduce these symptoms for most patients.
Dizziness and fatigue are reported but occur in 2–5% of users based on available data. These symptoms rarely require medication discontinuation but may affect daily activities.
Skin reactions, including rash and itching, occur infrequently but may necessitate switching to alternative anticoagulants. Drug-specific allergic reactions are rare but require immediate discontinuation and alternative anticoagulation strategies.
Cost Comparison & Coupons
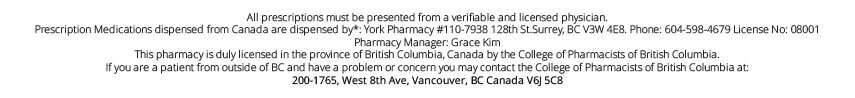
Understanding the true cost of anticoagulant therapy requires examining both retail prices and available discount programs. In the U.S., generic apixaban is not yet widely available as of 2025, so most patients pay the brand-name price of $478–$600 for a 30-day supply, depending on pharmacy and coupon use. In Canada, generic apixaban is available for $70–$100 per month.
Related Post – Is It Safe to Buy Eliquis from Canada? A Complete Guide for Fixed Income Retirees in America
Xarelto and Pradaxa maintain similar pricing to brand-name Eliquis, with 30-day supplies costing $500-$550. Savaysa prices are slightly lower at $480-$520 monthly. Warfarin remains the most economical option at approximately $4 for a 30-day supply, though patients must factor in INR monitoring costs.
Manufacturer co-pay cards can significantly reduce costs for commercially insured patients. Bristol-Myers Squibb offers the Eliquis Co-pay Card, which can reduce monthly costs to as low as $10 for eligible patients. Similar programs exist for other brand-name DOACs, though eligibility requirements and benefit limits vary.
Patient assistance programs (PAPs) provide free medications for qualifying low-income patients. Each manufacturer operates separate programs with different income requirements, typically ranging from 200-400% of federal poverty level. These programs require annual reapplication and physician participation.
Discount card programs like GoodRx, SingleCare, and others can provide 10-80% savings on prescription medications, particularly beneficial for uninsured patients or those in Medicare coverage gaps. These programs work at most pharmacies and don’t require pre-qualification.
How to Switch Anticoagulants Safely
Transitioning to Warfarin – Monitoring Requirements
Switching from DOACs to warfarin requires careful planning and monitoring to maintain therapeutic anticoagulation while avoiding excessive bleeding risk. The transition typically involves overlapping anticoagulation with parenteral agents like enoxaparin until warfarin reaches therapeutic INR levels.
The process begins with discontinuing the DOAC and initiating warfarin at appropriate starting doses, typically 5-10 mg daily for most patients. Simultaneously, patients receive enoxaparin or another low molecular weight heparin until INR levels reach 2.0-3.0 on consecutive measurements at least 24 hours apart.
INR monitoring frequency during warfarin initiation requires daily checks for the first 3-5 days, then every 2-3 days until stable therapeutic levels are achieved. This intensive monitoring period typically lasts 1-2 weeks, after which patients can transition to routine monitoring every 2-4 weeks.
Patient education becomes crucial during warfarin transitions. Patients must understand dietary restrictions, drug interactions, and the importance of consistent INR monitoring. Many patients benefit from warfarin education classes or comprehensive counseling sessions.
Switching to Other DOACs – Timing Considerations
Transitioning between different DOACs requires attention to timing and renal function to maintain appropriate anticoagulation. The general principle involves discontinuing the current DOAC and initiating the new agent at the time of the next scheduled dose.
For patients with normal kidney function, the switch can typically occur 12 hours after the last dose of a twice-daily DOAC or 24 hours after a once-daily agent. Patients with impaired renal function may require longer intervals between medications to allow adequate clearance.
Renal considerations become particularly important when switching anticoagulants. All DOACs require dose adjustments for kidney impairment, but the specific criteria and dose reductions vary among agents. Creatinine clearance calculations guide appropriate dosing decisions.
Close monitoring during the transition period helps identify any bleeding or thrombotic complications. Patients should receive clear instructions about when to seek medical attention and how to manage minor bleeding episodes during the switch.
Natural & Dietary Alternatives
Ginger, Turmeric, Garlic – Limited Clinical Evidence
Natural supplements marketed for cardiovascular health often claim anticoagulant properties, but robust clinical evidence supporting their use as eliquis alternatives remains limited. Ginger contains compounds like gingerols that may inhibit platelet aggregation, but studies showing clinically significant anticoagulant effects are lacking.
Turmeric’s active compound curcumin demonstrates anti-inflammatory properties and may affect blood clotting in laboratory studies. However, the bioavailability of curcumin is poor, and human studies haven’t established therapeutic anticoagulant effects comparable to prescription medications.
Garlic supplements contain compounds that may influence blood clotting, but clinical trials haven’t demonstrated consistent anticoagulant effects. Additionally, garlic can interact with prescription anticoagulants, potentially increasing bleeding risk when used concurrently.
The lack of standardization in natural supplement preparations makes it impossible to ensure consistent dosing or effects. Unlike FDA-approved medications, dietary supplements don’t undergo rigorous testing for safety and efficacy. Patients considering natural blood thinners should discuss these options with healthcare providers and never discontinue prescribed anticoagulants without medical supervision.
Insurance, Patient Support & Saving Strategies
Navigating insurance coverage for anticoagulants requires understanding formulary restrictions, prior authorization requirements, and available assistance programs. Many insurance plans prefer generic medications or specific brand-name agents, requiring patients to try preferred options before covering alternatives.
State pharmaceutical assistance programs provide additional resources for eligible patients. Programs like PACE (Pharmaceutical Assistance Contract for the Elderly) in Pennsylvania and similar initiatives in other states offer prescription drug coverage for seniors and disabled individuals who don’t qualify for other assistance programs.
Medicare Part D coverage for anticoagulants varies by plan, with some plans requiring step therapy or prior authorization. The Medicare coverage gap (donut hole) can create temporary high out-of-pocket costs, making manufacturer assistance programs particularly valuable for Medicare beneficiaries.
Pharmaceutical company patient assistance programs typically provide the most comprehensive support for qualifying patients. Bristol-Myers Squibb’s Patient Assistance Foundation, Bayer’s Patient Assistance Program, and similar initiatives from other manufacturers can provide free medications for patients meeting income requirements.
Frequently Asked Questions
Is generic apixaban as effective as brand-name Eliquis?
Yes, generic apixaban must demonstrate bioequivalence to Eliquis, meaning it delivers the same amount of active ingredient to your bloodstream at the same rate. The FDA requires generic medications to have identical therapeutic effects as brand-name versions.
Can I switch between different blood thinners on my own?
No, switching anticoagulants requires medical supervision to ensure proper timing and dosing. Improper transitions can lead to dangerous blood clots or bleeding complications. Always consult your healthcare provider before making changes.
How much money can I save with anticoagulant coupons?
Savings vary significantly depending on your insurance status and the specific program. Manufacturer co-pay cards can reduce costs to $10-$25 monthly for commercially insured patients, while patient assistance programs may provide free medications for qualifying low-income individuals.
Are natural blood thinners safe alternatives to prescription medications?
Natural supplements lack the clinical evidence supporting prescription anticoagulants and aren’t appropriate substitutes for FDA-approved medications in patients requiring anticoagulation for conditions like atrial fibrillation or blood clots.
What should I do if I can’t afford my blood thinner?
Contact your healthcare provider immediately to discuss alternatives. Options may include generic versions, manufacturer assistance programs, state pharmacy assistance programs, or switching to more affordable alternatives like warfarin with appropriate monitoring.
How do I know which blood thinner is right for me?
The choice depends on multiple factors including your medical condition, kidney function, other medications, bleeding risk, and ability to comply with monitoring requirements. Your healthcare provider will consider all these factors to recommend the most appropriate option.
Conclusion & Next Steps
The landscape of eliquis alternatives offers multiple options for patients seeking effective and affordable anticoagulation. Generic apixaban provides the most direct cost savings while maintaining identical efficacy to brand-name Eliquis. Other DOAC alternatives like Xarelto, Pradaxa, and Savaysa offer different dosing schedules and safety profiles that may better suit individual patient needs.
Warfarin remains a highly effective and economical choice for patients who can manage INR monitoring and dietary considerations. The dramatic cost difference – approximately $4 versus $550 monthly – makes warfarin particularly attractive for uninsured patients or those facing high co-payments.
For patients who prefer to continue with Eliquis or generic apixaban due to their proven safety profile and convenience, exploring affordable pharmacy options becomes essential. When you’re ready to buy Eliquis at reduced costs, PrescriptionPoint.com offers significant savings on Eliquis and other anticoagulants, providing access to FDA-approved medications at substantially reduced prices. This trusted online pharmacy platform connects Americans with licensed pharmacies, ensuring medication authenticity while delivering meaningful cost savings that can make the difference between affording treatment and going without.
Patient assistance programs, manufacturer co-pay cards, and discount programs can significantly reduce the financial burden of anticoagulant therapy. Combining these resources with affordable pharmacy options like PrescriptionPoint.com often reveals multiple pathways to accessing necessary medications without compromising household budgets.
The decision to switch anticoagulants should always involve comprehensive discussion with healthcare providers. Factors including medical history, kidney function, drug interactions, bleeding risk, and lifestyle considerations all influence the optimal choice for individual patients. However, cost should never force patients to compromise on medically appropriate therapy when affordable alternatives exist.
Moving forward, patients should work closely with their healthcare teams to evaluate both clinical and cost considerations when selecting anticoagulants. Exploring resources like PrescriptionPoint.com for medication savings, while maintaining regular monitoring and open communication with providers, ensures safe, effective anticoagulation without financial hardship. The goal remains preventing dangerous blood clots while maintaining quality of life and financial stability through smart healthcare purchasing decisions.
References
- CDC.gov. (2025). Data and Statistics on Venous Thromboembolism
- Wikipedia.org. (2025). Pulmonary embolism
- CDC.gov. (2024). About Atrial Fibrillation
- VeryWellHealth.com. (2023). What Is Deep Vein Thrombosis?
- Bms.com. (2025). Key facts
- Accessdata.fda.gov. (2021). Prescribing Information
- Singlecare.com. (2025). What tier drug is Eliquis?
- Healthline.com. (2024). Is Eliquis Covered by Medicare?
- Singlecare.com. (2024). Eliquis interactions to avoid
- Tctmd.com. (2019). FDA Approves Two Generic Versions of Apixaban
- Brieflands.com. (2025). Pharmacokinetics and Bioequivalence of Two Formulations of Apixaban Tablets: A Double-Blind, Single-Dose, Crossover Study in Healthy Subjects
- Dataintelo.com. (2024). Apixaban API Market
- Singlecare.com. (2023). Eliquis generic availability, cost, and dosage
- Rxlist.com. (2021). Apixaban
- Janssenlabels.com. (2023). Patient Counselling Information
- Goodrx.com (2024). 7 Xarelto Side Effects You Should Know About
- Mayoclinic.org. (2025). Rivaroxaban (oral route)
- Wikipedia.org. (2025). Dabigatran
- Drugwatch.com. (2025). Blood Thinners.
- Pubmed.ncbi.nlm.nih.gov. (2016). Safety Signal Evaluation of a Risk of Syncope and Dizziness Not Related to Bleeding or Stroke in Direct Oral Anticoagulant-treated Patients
- Eurannallergyimm.com. (2019). Delayed hypersensitivity to new oral anticoagulants. Demonstration of cross reactivity for the drug category and definition of non-irritant concentrations for patch tests
- Singlecare.com. (2025). How much do blood thinners cost?
- Medicalnewstoday.com. (2023). Eliquis (apixaban) and cost
- Singlecare.com. (2025). Eliquis Coupons
- Goodrx.com (2025). Apixaban
- Ahajournals.org. (2020). Direct Oral Anticoagulant Use: A Practical Guide to Common Clinical Challenges
- Southdenver.com. Switching To and From Various Anticoagulants
- Gov.bc.ca. (2023). Direct Oral Anticoagulants (DOACs)
- National Library of Medicine. (2023). Functional bioactive compounds in ginger, turmeric, and garlic
- Jhrlmc.com. (2024). Exploring the Cardio-Protective Effect of Bioactive Compounds Present in Ginger, Garlic, and Turmeric
- Journals.sagepub.com. (2024). Efficacy of Phytopharmaca (Cinnamon, Turmeric, Ginger and Garlic) as an Adjuvant in Rheumatoid Arthritis Management: A Systematic Review and Meta-Analysis
- Sciencedirect.com. (2017). Old and new oral anticoagulants: Food, herbal medicines and drug interactions
- National Library of Medicine. (2023). Functional bioactive compounds in ginger, turmeric, and garlic
- Wiley.com. (2018). Effects of Garlic, Onion, Ginger, and Turmeric on Platelet Function
- Irjet.net. (2019). Health benefits and possible Risks of Turmeric, Garlic and Ginger: A short review
- Milliman.com. (2025). Potential impact of formulary restrictions on anticoagulants in the Post- Maximum Fair Price (MFP) Part D Market
- Ajmc.com. (2022). Formulary Restrictions and Stroke Risk in Patients With Atrial Fibrillation
- Medicalnewstoday.com. (2022). Xarelto vs. Eliquis
- Goodrx.com. (2023). Plavix vs. Eliquis: 7 Things to Know When Comparing These Blood Thinners
- Ti.ubc.ca. (2024). Apixaban is safer and more effective than rivaroxaban for non-valvular atrial fibrillation
- Fda.gov. (2020). 2019 First Generic Drug Approvals